Bacteria vs. Viruses: Key Differences and Similarities Explained
Table of Contents
I. Introduction
Understanding the fundamental distinctions and connections between bacteria and viruses is essential for grasping their respective roles in health and disease. These two entities, while often grouped together in casual discussions about pathogens, possess stark differences in structure, reproduction, and treatment. Bacteria are unicellular organisms that can live independently, while viruses are acellular entities that require a host to multiply and survive. Their variances have significant implications for healthcare, as bacterial infections can often be treated with antibiotics, whereas viral infections necessitate different therapeutic approaches. In addition, certain viruses can lead to chronic health issues, which underscores the importance of thorough research into their interaction with human biology. To aid in this understanding, a Venn diagram illustrating these differences and similarities effectively encapsulates their unique characteristics and shared capabilities in causing disease, providing a valuable visual aid for students and researchers alike .
A. Definition of bacteria and viruses
Bacteria and viruses represent two fundamentally distinct biological entities that play significant roles in health and disease. Bacteria are unicellular microorganisms characterized by their cellular structure, which allows them to thrive in a variety of environments. They possess a complete set of genetic material and can reproduce independently through a process known as binary fission. In contrast, viruses are much smaller and are not considered living organisms; they require a host cell for replication and are made up of genetic material encased in a protein shell, lacking cellular structures. The interaction between these two types of pathogens can significantly impact human health, as each can cause a wide range of diseases. A Venn diagram, such as that seen in , effectively illustrates the key differences and similarities between bacteria and viruses, providing a visual representation that underscores their unique characteristics and interactions in the context of infectious diseases.
| Type | Definition | Characteristics |
| Bacteria | Single-celled microorganisms that can exist independently, symbiotically, or as parasites. They have a simple cellular structure without a nucleus. | Prokaryotic, can reproduce independently, can be beneficial or pathogenic, have cell walls, and can be found in various environments. |
| Viruses | Microscopic infectious agents that require a host cell to replicate and propagate. They are not considered living organisms. | Acellular, require a host for reproduction, generally pathogenic, lack cellular structures, and can infect all types of life forms. |
Bacteria vs. Viruses: Definitions and Characteristics
B. Importance of understanding the differences and similarities
Understanding the differences and similarities between bacteria and viruses is pivotal for various disciplines, particularly in the fields of medicine and microbiology. This knowledge not only informs treatment strategies but also enhances the development of vaccines and therapeutics. For instance, the distinct biological characteristics of bacteria—such as being living organisms capable of reproduction—contrast sharply with the non-living nature of viruses, which require a host cell for replication. Such contrasts are visually encapsulated in Venn diagrams, such as , which highlight both unique traits and shared capabilities, such as disease causation. Moreover, understanding these differences and similarities aids public health initiatives aimed at disease prevention, improving layperson awareness regarding the appropriate responses to infections. The implications of these insights extend to antibiotic usage and the management of viral infections, underscoring the critical need for accurate differentiation in clinical and public health contexts.
| Characteristic | Bacteria | Viruses |
| Cell Structure | Prokaryotic (single-celled) | Acellular (not composed of cells) |
| Living Status | Living organisms | Non-living entities |
| Reproduction | Reproduce asexually through binary fission | Reproduce only within a host cell |
| Antibiotic Response | Can be treated with antibiotics | Antibiotics are ineffective; antiviral medications are used |
| Size | Typically 0.5 to 5 micrometers | Typically 20 to 300 nanometers |
| Genetic Material | Contain both DNA and RNA | Contain either DNA or RNA, not both |
| Examples | Escherichia coli, Streptococcus | Influenza, HIV |
Bacteria vs. Viruses: Key Differences and Similarities
II. Key Differences Between Bacteria and Viruses
The fundamental distinctions between bacteria and viruses lie in their structural characteristics and biological functions. Bacteria are unicellular, prokaryotic organisms that possess a complex cellular structure, including a cell wall, cell membrane, and genetic material organized in a single chromosome. They are capable of independent life, reproduction through binary fission, and can be treated with antibiotics. In contrast, viruses are significantly smaller, non-cellular entities made up of genetic material encased in a protein coat, lacking the cellular machinery necessary for metabolism and reproduction. They require a living host cell to replicate, effectively hijacking the hosts cellular mechanisms to produce new viral particles. This critical difference is graphically represented in , which delineates the key attributes of both bacteria and viruses, emphasizing their respective roles in health and disease. Understanding these fundamental differences is essential for developing targeted medical treatments and public health strategies.
| Characteristic | Bacteria | Viruses |
| Cellular Structure | Single-celled organisms with a complex structure including cell walls and membranes. | Acellular entities, consisting of genetic material encased in a protein coat. |
| Bacteria | Reproduce asexually through binary fission. | Cannot reproduce independently; they hijack host cells to replicate. |
| Bacteria | Considered living organisms as they possess cellular machinery. | Considered non-living as they do not have cellular functions on their own. |
| Bacteria | Generally larger (0.5 – 5 micrometers). | Much smaller (20 – 300 nanometers). |
| Bacteria | Often treated with antibiotics. | Usually treated with antiviral medications; antibiotics are ineffective. |
| Bacteria | Salmonella, E. coli, Streptococcus. | Influenza, HIV, SARS-CoV-2. |
Key Differences Between Bacteria and Viruses
A. Structure and Composition
The structural composition of bacteria and viruses reveals fundamental differences that underscore their distinct biological roles. Bacteria, being unicellular organisms, possess a complex structure characterized by a cell wall, cell membrane, cytoplasm, and genetic material organized in a singular circular DNA molecule. This composition enables bacteria to maintain metabolic functions and reproduction independently. In contrast, viruses are acellular entities that consist of a core of genetic material—either DNA or RNA—enclosed in a protein coat known as a capsid, and, in some cases, an additional lipid envelope. Unlike bacteria, viruses are incapable of independent reproduction and must hijack a host cells machinery to replicate. This critical distinction in structure is effectively illustrated in the Venn diagram , which succinctly captures both the unique attributes and shared characteristics of bacteria and viruses, providing a foundational understanding of their compositions and the implications for their roles in health and disease.
| Type | Size (in micrometers) | Cell Structure | Genetic Material | Cell Membrane | Cell Wall | Reproduction | Living/Non-Living |
| Bacteria | 0.5 – 5.0 | Prokaryotic | Circular DNA | Yes | Present (Peptidoglycan) | Binary Fission | Living |
| Viruses | 20 – 300 | Acellular | DNA or RNA (linear or circular) | No | Absent | Requires a host cell | Non-Living |
Bacteria vs. Viruses: Structure and Composition Comparison
B. Methods of Reproduction
The methods of reproduction differentiate bacteria and viruses in fundamental ways that impact their biological behaviors and ecological roles. Bacteria predominantly reproduce asexually through binary fission, a process where a single bacterial cell divides into two genetically identical daughter cells, thereby promoting rapid population growth. This mode is efficient in stable environments, allowing bacteria to colonize niches quickly. Conversely, viruses lack independent cellular machinery and must hijack the hosts cellular processes to replicate. Their reproduction involves complex life cycles, such as the lytic and lysogenic cycles, where they rely on the hosts cellular machinery to produce new virions after infection. The intricate nature of viral reproduction is illustrated in the depiction of lytic and lysogenic strategies, highlighting the variability in their approaches compared to the relatively straightforward binary fission of bacteria . Understanding these reproduction methods is critical to developing targeted treatments for infections caused by these two distinct groups.
| Organism Type | Reproduction Method | Time for Reproduction | Genetic Variation | Examples |
| Bacteria | Asexual (Binary Fission) | 20 minutes to several hours | Low (Mutation during replication) | Escherichia coli, Staphylococcus aureus |
| Viruses | Assexual (Host Cell Lysis or Budding) | 1 hour to several days | High (Recombination and Mutation) | Influenza virus, Human Immunodeficiency Virus (HIV) |
Methods of Reproduction in Bacteria and Viruses
C. Response to Antibiotics
Antibiotic response varies significantly between bacteria and viruses, fundamentally influencing treatment approaches for infections. Bacteria, which are living organisms, can be targeted by antibiotics that disrupt their cell wall synthesis or inhibit protein production, leading to cell death or growth cessation. This specificity is crucial as many antibiotics are designed to harness unique bacterial structures, ensuring selective toxicity. In contrast, viruses lack the cellular machinery necessary for replication, rendering conventional antibiotics ineffective, as these agents are not considered living cells. The response to treatment in viral infections often relies on antiviral medications that inhibit viral replication or bolster the immune systems defenses. The implications of this dichotomy are visually represented in , which categorically outlines how bacteria can be effectively treated with antibiotics, while viruses require a distinctly different therapeutic approach. Understanding these fundamental differences is essential for developing effective clinical strategies in managing infectious diseases.
| Type | Response to Antibiotics | Example of Antibiotics | Resistance Occurrence |
| Bacteria | Most are susceptible | Penicillin, Amoxicillin | Rising, approximately 300,000 infections in the U.S. annually |
| Viruses | Not susceptible | Antiviral medications (e.g., Oseltamivir) | N/A |
| Bacterial Infections (e.g., MRSA) | Resistance present | Vancomycin | Reported in 56% of isolates in some regions |
| Viral Infections (e.g., HIV) | N/A | ART (Antiretroviral Therapy) | N/A |
Response to Antibiotics in Bacteria and Viruses
D. All other differences
In examining the myriad differences between bacteria and viruses, it becomes clear that their structural and functional distinctions extend beyond mere size and classification. Bacteria are prokaryotic cells, characterized by their complex cell walls and ability to thrive independently, engaging in metabolic processes that sustain them autonomously. In contrast, viruses embody a more enigmatic existence, consisting only of a protein coat and genetic material, and relying entirely on the hosts cellular machinery for replication. This fundamental disparity influences their treatment; while antibiotics can effectively target bacterial infections, they have no impact on viral maladies. Additionally, the methods of transmission and infection differ significantly: bacteria can proliferate through asexual reproduction in various environments, while viruses require precise mechanisms to hijack host cells, as illustrated in the replication cycle depicted in the image . Understanding these differences is essential for developing effective medical responses and public health strategies against diverse infectious agents.
| Characteristic | Bacteria | Viruses |
| Cell Type | Prokaryotic | Acellular |
| Size | Larger (0.5 – 5 micrometers) | Smaller (20 – 400 nanometers) |
| Reproduction | Binary fission | Requires host cell |
| Living Status | Living organisms | Non-living entities |
| Antibiotic Sensitivity | Can be treated with antibiotics | Not affected by antibiotics |
| Genetic Material | DNA (circular) | DNA or RNA (linear or circular) |
Differences Between Bacteria and Viruses
III. How to Identify Bacterial vs. Viral Infections
Differentiating between bacterial and viral infections is crucial for accurate diagnosis and treatment, as the management strategies for each type of infection vary significantly. Bacteria are living microorganisms that can reproduce independently, while viruses require a host cell to replicate, rendering them non-living entities in isolation. Clinically, bacterial infections often exhibit symptoms like localized pain, swelling, and pus formation, whereas viral infections tend to present with systemic symptoms such as fever, fatigue, and muscle aches. Laboratory tests, including cultures and PCR analyses, can aid in identification—bacteria will grow on culture plates, while viruses typically require specialized assays for detection. A comprehensive understanding of these distinctions is further enhanced by visual tools such as , which succinctly compare and contrast bacteria and viruses, highlighting their biological characteristics and implications for human health. Such distinctions are pivotal not only for treatment but also for understanding public health concerns related to infectious diseases.
| Characteristic | Bacterial Infection | Viral Infection |
| Type of Pathogen | Bacteria | Virus |
| Cell Structure | Single-celled, prokaryotic | Non-cellular, requires host cell |
| Reproduction | Reproduces independently through binary fission | Reproduces only within a host cell |
| Treatment | Antibiotics are effective | Antibiotics are ineffective; antiviral medications may be used |
| Symptoms | Localized pain, fever, pus, swelling | Fever, fatigue, muscle aches, cough |
| Examples | Strep throat, tuberculosis, urinary tract infections | Influenza, COVID-19, common cold |
Bacterial vs. Viral Infections Identification
A. Common Symptoms
When examining the common symptoms associated with bacterial and viral infections, certain overlapping features emerge, although the underlying causes differ significantly. Both types of pathogens can elicit responses such as fever, fatigue, and inflammation, which are the body’s natural defenses against infection. For instance, bacterial infections often present with localized symptoms such as pus formation or swelling, while viral infections may lead to systemic symptoms like muscle aches and generalized weakness. Additionally, respiratory symptoms such as sore throat and cough are frequently observed in both types of infections, complicating initial diagnosis. Moreover, while both infections can cause gastrointestinal disturbances, bacterial infections may be more likely to result in severe diarrhea or vomiting, highlighting an important distinction in symptomatology. Understanding these common symptoms can aid in differentiation and foster more effective treatment strategies, as the appropriate response to each infection type can vary significantly. Thus, a nuanced appreciation of these symptoms is essential in clinical practice.
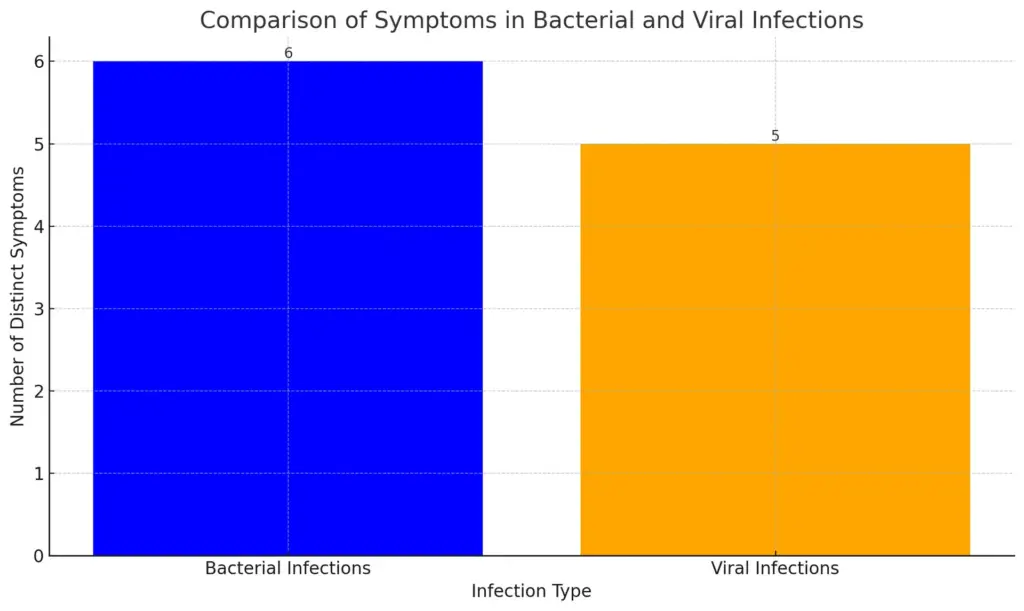
This bar chart compares the distinct symptoms associated with bacterial and viral infections. It shows that bacterial infections are represented by six distinct symptoms, while viral infections have five distinct symptoms, indicating a slight variation in the symptom representation between the two categories.
B. Diagnostic Methods
In the realm of microbiology, accurate diagnostic methods are crucial for distinguishing between bacterial and viral infections, each of which necessitates different treatment strategies. Traditional cultures, serological tests, and modern molecular techniques such as polymerase chain reaction (PCR) are frequently employed in clinical settings to identify pathogens. Culturing bacteria allows for the examination of their growth characteristics and susceptibility to antibiotics, thereby guiding effective treatment plans. Conversely, viruses, being non-living entities, require more sophisticated techniques; for instance, the detection of viral RNA through PCR offers rapid and sensitive diagnosis. The life cycle of such viruses may also be portrayed visually to enhance understanding of their pathogenic mechanisms, as illustrated in relevant diagrams . Ultimately, the choice of diagnostic method is integral to epidemiological surveillance and public health interventions, ensuring that appropriate measures are taken to contain infectious diseases and prevent their transmission.
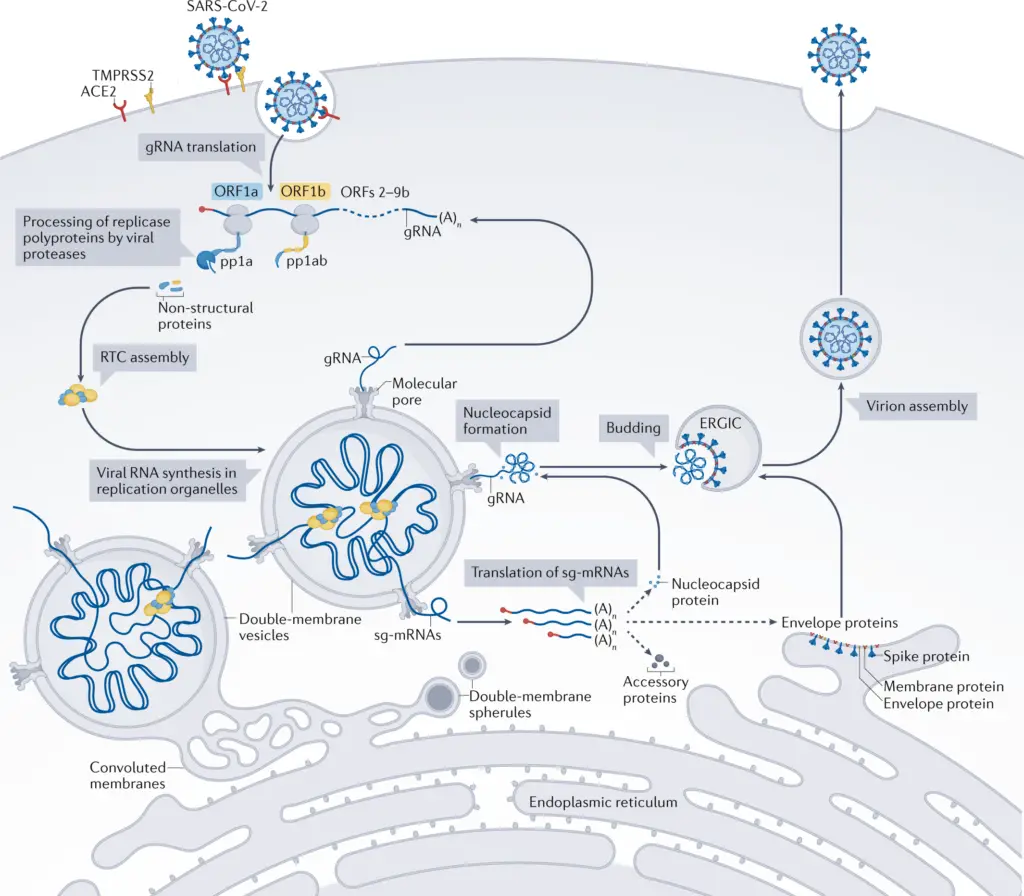
IMAGE – Replication cycle of SARS-CoV-2 highlighting key molecular processes. (The image presents a detailed diagram illustrating the replication cycle of SARS-CoV-2, emphasizing key molecular and cellular processes involved in viral propagation. It includes annotations for various components such as the viral RNA translation mechanism, processing of replicase polyproteins, assembly of non-structural proteins, and the role of specific proteins like TMPRSS2 and ACE2. Key stages like viral RNA synthesis, nucleocapsid formation, and virion assembly within the endoplasmic reticulum and cytoplasmic organelles are also highlighted. This diagram serves as a valuable resource for understanding the molecular biology of coronaviruses and the specific steps of SARS-CoV-2 infection and replication, which are crucial for both fundamental virology and applied research in vaccine development and therapeutics.)
IV. Differences in life cycles between bacteria and viruses
The life cycles of bacteria and viruses exhibit fundamental differences that underscore their unique biological natures. Bacteria, as unicellular organisms, reproduce through a process known as binary fission, whereby one bacterial cell divides into two identical daughter cells, facilitating a relatively rapid population increase under favorable conditions. In contrast, viruses cannot replicate independently; they must invade a host cell to hijack its machinery for reproduction. Upon entry, a virus may undertake either a lytic or lysogenic life cycle, where the former culminates in immediate host cell lysis and the release of viral progeny, while the latter involves integration into the host genome, remaining dormant until conditions favor active replication. This crucial distinction in reproductive strategies illustrates the critical role that host cell interaction plays in viral life cycles, compared to the autonomous reproductive capabilities of bacteria. To visualize these differences effectively, the comprehensive diagram of the lytic and lysogenic cycles found in serves to clarify these contrasting processes.
| LifecycleStage | Bacteria | Viruses |
| Attachment | Generally have a rigid cell wall and can attach to surfaces via pili or fimbriae. | Attach to specific receptors on the host cell surface using viral proteins. |
| Entry | May enter host cells directly or through the secretion of enzymes to degrade host tissues. | Enter host cells by fusion with cell membrane or endocytosis. |
| Replication | Replicate independently by binary fission, duplicating their DNA and cell components. | Hijack the host cell’s machinery to replicate their genetic material and produce viral proteins. |
| Assembly | New cells are formed and assembled naturally within the cell. | New viral particles are assembled from replicated genetic material and proteins inside the host cell. |
| Release | Divide into two or more daughter cells, releasing them into the environment. | Exit the host cell either by lysis (bursting the cell) or budding off from the cell membrane. |
Differences in Life Cycles Between Bacteria and Viruses
V. Impact on Human Health
The impact of bacteria and viruses on human health is profound and multifaceted, playing crucial roles in both disease causation and human physiology. Bacteria, which are generally larger and can proliferate independently, can be beneficial or harmful; they reside in the human microbiome and play essential roles in metabolism and immune function. Conversely, viruses, smaller entities that require a host cell to reproduce, are often associated with acute diseases like influenza and HIV, which can lead to severe health complications or death. The understanding of these microorganisms is vital not only for the development of treatments and vaccines but also for public health strategies aimed at controlling infectious diseases. As scientists continue to unravel the complexities of bacterial and viral interactions with human cells, it becomes increasingly clear that these tiny organisms significantly shape the landscape of human health. This intricate dance between host and pathogen emphasizes the need for comprehensive studies to inform effective clinical and preventive measures, as illustrated in the image .
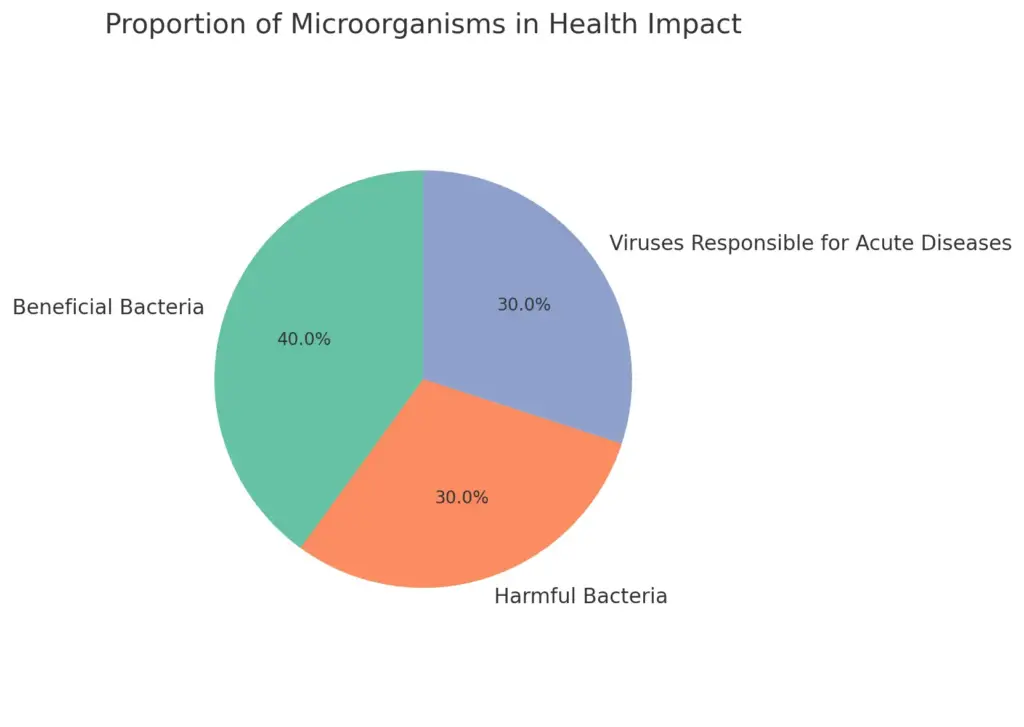
This pie chart represents the proportion of beneficial bacteria, harmful bacteria, and viruses responsible for acute diseases. Beneficial bacteria make up 40 percent of the impact, while harmful bacteria and viruses each contribute 30 percent. This visualization highlights the complex roles these microorganisms play in human health.
A. Bacterial infections and their treatments
Bacterial infections pose significant health challenges, necessitating effective treatment strategies tailored to combat these pathogens. Unlike viruses, bacteria are living organisms capable of independent reproduction, which influences their treatment. Antibiotics are the primary method for treating bacterial infections, functioning by targeting specific bacterial processes such as cell wall synthesis or protein production without harming human cells. The emergence of antibiotic resistance, however, complicates these treatments, as some bacteria evolve mechanisms to survive antibiotic exposure, leading to infections that are increasingly difficult to treat. Understanding the life cycles and pathogenic mechanisms of bacteria is vital in developing new therapeutic approaches. For instance, visual tools such as effectively illustrate the differences between bacteria and viruses, aiding in the understanding of how treatment methods differ accordingly. Consequently, ongoing research is crucial to enhance our arsenal against bacterial infections and address the pressing issue of antibiotic resistance tangibly.
| Infection | Causative Agent | Common Symptoms | Treatment | Recovery Time |
| Strep Throat | Streptococcus pyogenes | Sore throat, fever, headache | Penicillin or Amoxicillin | 3-7 days |
| Urinary Tract Infection (UTI) | Escherichia coli | Painful urination, frequent urge to urinate, cloudy urine | Nitrofurantoin or Trimethoprim/Sulfamethoxazole | 1-3 days |
| Pneumonia | Streptococcus pneumoniae | Cough, fever, difficulty breathing | Azithromycin or Amoxicillin | 1-3 weeks |
| Tuberculosis | Mycobacterium tuberculosis | Cough, weight loss, night sweats | Isoniazid, Rifampin, Ethambutol, Pyrazinamide | 6-12 months |
| Bacterial Meningitis | Neisseria meningitidis | Fever, headache, stiff neck | Ceftriaxone or Vancomycin | 2 weeks to several months |
Bacterial Infections and Treatments
B. Viral infections and their treatments
Understanding viral infections and their treatments requires a nuanced appreciation of the complexities inherent in viral biology. Unlike bacteria, viruses rely entirely on host cells for replication, which complicates therapeutic strategies. Antiviral treatments often target specific stages of the viral life cycle, such as entry, replication, and assembly, thereby minimizing damage to host cells. This contrasts sharply with bacterial infections, where antibiotics can effectively disrupt vital processes without harming human cells. For instance, the lytic cycle of viruses, as depicted in , highlights the aggressive nature of viral replication and subsequent host cell destruction, underscoring the urgency to develop targeted antiviral therapies. Furthermore, the development of monoclonal antibodies and novel vaccines has emerged as promising strategies to combat viral infections, rendering them preventable and treatable. As we continue to explore these interventions, it becomes evident that the distinctions between viral and bacterial infections not only inform treatment approaches but also dictate the ongoing evolution of public health strategies.
| Virus | Incidence (per 100,000 people) | Mortality Rate (%) | Treatment |
| Influenza | 220 | 0.1 | Antiviral medications (e.g., oseltamivir) |
| HIV | 13.2 | 0.7 | Antiretroviral therapy (ART) |
| COVID-19 | 1350 | 1.8 | Vaccines, antiviral medications (e.g., remdesivir) |
| Hepatitis B | 6.4 | 0.7 | Antiviral medications (e.g., tenofovir) |
| Herpes Simplex Virus | 200 | 0.1 | Antiviral medications (e.g., acyclovir) |
Viral Infections and Treatments
C. Role of antibiotics and antivirals in managing infections
The roles of antibiotics and antivirals in managing infections highlight fundamental differences between bacterial and viral pathogens. Antibiotics, designed specifically to combat bacterial infections, work by targeting critical bacterial processes such as cell wall synthesis or protein translation, effectively halting bacterial growth and replication. In contrast, antivirals target specific stages of viral infection cycles, preventing viruses from entering host cells or inhibiting their replication. Understanding these mechanisms is crucial, as improper use of antibiotics can lead to antibiotic resistance, a growing concern in global health. Furthermore, the efficacy of antivirals is particularly prominent in the treatment of viral infections like influenza or HIV, where timely administration can significantly improve patient outcomes. The complexities of these treatments underscore the necessity for accurate diagnosis and tailored therapeutic strategies. To visually encapsulate these differences, effectively summarizes the key distinctions between bacteria and viruses, reinforcing the importance of employing appropriate infection management strategies.
| Type | Example | Target Infections | Effectiveness Rate (%) | Year of Study | Source |
| Antibiotic | Amoxicillin | Bacterial infections (e.g., strep throat, pneumonia) | 85 | 2023 | CDC |
| Antiviral | Oseltamivir (Tamiflu) | Influenza virus | 70 | 2023 | WHO |
| Antibiotic | Ciprofloxacin | Urinary tract infections, certain gastrointestinal infections | 90 | 2023 | PubMed |
| Antiviral | Acyclovir | Herpes virus infections | 80 | 2023 | NIH |
Antibiotics and Antivirals Effectiveness
VI. Conclusion
In conclusion, understanding the intricate differences and similarities between bacteria and viruses is essential for advancing public health, scientific research, and effective treatment strategies. While both microorganisms can cause significant health issues, their fundamental distinctions—such as structure, reproduction methods, and treatment responses—underscore the necessity for targeted approaches in medical practice. For instance, as illustrated in the Venn diagram , the contrasting characteristics of these pathogens highlight the complexities involved in diagnosing and treating infections. Additionally, recognizing these differences helps inform vaccine development and appropriate use of antibiotics, which are effective against bacteria but not against viruses. The ongoing research into their interactions further illuminates their roles in ecosystems, disease propagation, and even potential therapeutic applications. Ultimately, this knowledge empowers healthcare professionals and the public to make informed decisions, fostering a more nuanced understanding of disease mechanisms and prevention.
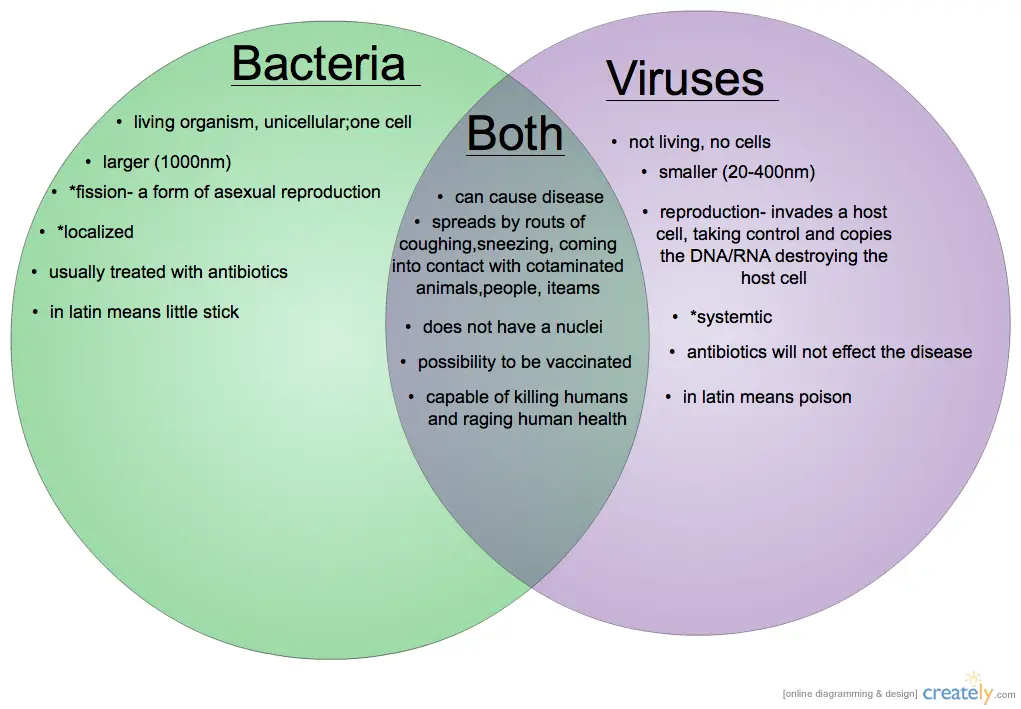
IMAGE – Comparison of Bacteria and Viruses in Microbiology
REFERENCES
- Board on Health Promotion and Disease Prevention. ‘The Future of the Public’s Health in the 21st Century.’ Institute of Medicine, National Academies Press, 2/1/2003
- Paul Auerbach. ‘Enviromedics.’ The Impact of Climate Change on Human Health, Jay Lemery, Rowman & Littlefield, 10/20/2017
- Jennifer Louten. ‘Essential Human Virology.’ Academic Press, 5/28/2022
- Alessandro Minelli. ‘The Biology of Reproduction.’ Giuseppe Fusco, Cambridge University Press, 10/10/2019
- R. Hakenbeck. ‘Bacterial Cell Wall.’ J.-M. Ghuysen, Elsevier, 2/9/1994
- William Stillwell. ‘An Introduction to Biological Membranes.’ Composition, Structure and Function, Elsevier, 6/30/2016
- Samuel Reid. ‘Academic Writing Skills 2 Student’s Book.’ Peter Chin, Cambridge University Press, 12/15/2011
- Cesar V. Teague. ‘Plan B: 5 Differences That Make a Difference in Your Small/Home Business.’ 5 Differences That Make a Difference in Your Small/Home Business, Xlibris Corporation, 8/9/2011
- Alistair McCleery. ‘An Introduction to Book History.’ David Finkelstein, Routledge, 3/13/2006
Image References:
- Image: Replication cycle of SARS-CoV-2 highlighting key molecular processes., Accessed: 2025.https://media.springernature.com/full/springer-static/image/art%3A10.1038%2Fs41580-021-00432-z/MediaObjects/41580_2021_432_Fig1_HTML.png
- Image: Comparison of Bacteria and Viruses in Microbiology, Accessed: 2025.https://ultrapressurecleaning.com/wp-content/uploads/2020/04/Bacteria-vs-Virus-Venn-Diagram.png
