How the Immune System Fights Bacteria and Viruses: Innate and Adaptive Defenses
Table of Contents
I. Introduction to the Immune System
The immune system is the body’s defense against germs, like bacteria and viruses. It can be divided into two main parts: innate and adaptive immunity. Innate immunity is the first defense and reacts right away but does not target specific germs. It includes physical barriers such as skin and mucous membranes, along with cells like phagocytes and natural killer cells that quickly respond to infections. On the other hand, adaptive immunity takes longer to develop but offers a specific and long-lasting defense. This involves T and B lymphocytes that target specific germs they have encountered. The way these two immune parts work together shows how complicated the immune response is, as shown in [citeX], which visually explains how both processes connect to help the body fight infections. Knowing about this dual system is important for understanding how the immune system works as a whole.
A. The Importance of Immunity
Immunity is very important for protecting health by creating a defense system against germs like bacteria and viruses. The immune system has two main parts: innate and adaptive. The innate immune response is the first to react, quickly responding to infections with barriers and immune cells. The adaptive immune response takes longer to develop but provides long-lasting defense through memory cells and specific antibodies. This two-part approach not only helps to deal with immediate threats but also prepares the body for future encounters with the same germs. It builds a strong system that allows the body to recognize and remember past infections, leading to better responses in the future. The significance of this immune interaction is shown in [citeX], which demonstrates how immune responses change over time, emphasizing how innate responses prepare for adaptive immunity that targets various germs. Knowing how immunity works is key to creating vaccines and treatment plans, which improves public health outcomes. By understanding how these systems work together, researchers and healthcare providers can tackle public health issues, including new infectious diseases and possible outbreaks. Furthermore, raising awareness about the importance of a strong immune system through good nutrition, exercise, and healthy habits is essential for encouraging people to take charge of their health. Investing time in learning more about immunity can help build a stronger population that can effectively face health threats.
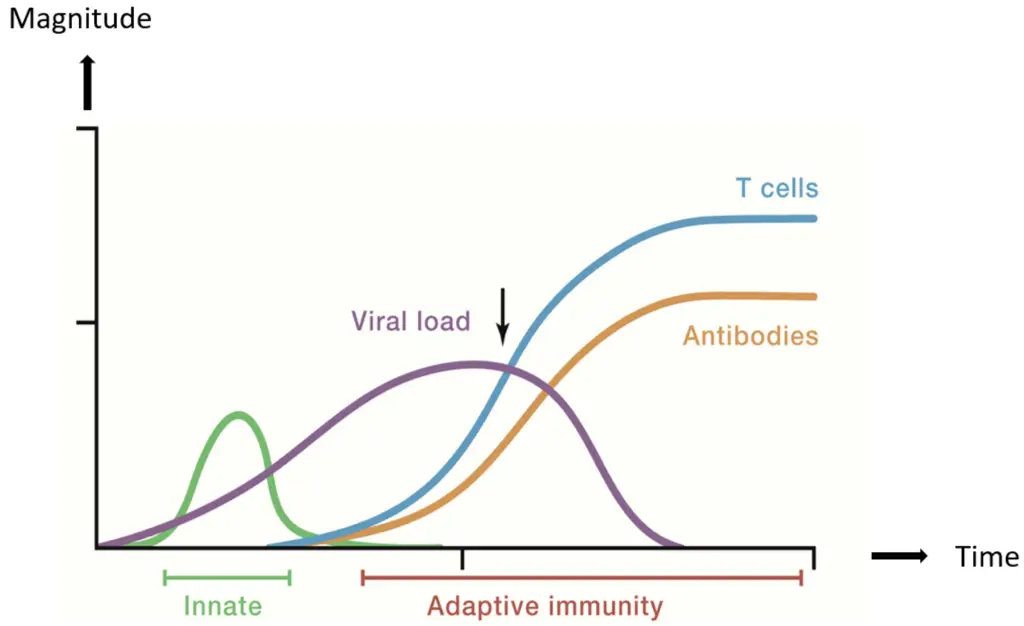
Graphical representation of immune response over time. (The image depicts a graphical representation of the immune response over time, illustrating the interplay between innate and adaptive immunity. The y-axis denotes ‘Magnitude,’ while the x-axis indicates ‘Time.’ There are four curves represented: ‘Innate’ immunity (green), ‘Viral load’ (purple), ‘Antibodies’ (orange), and ‘T cells’ (blue). The graph demonstrates how the viral load peaks initially before a response from the innate immune system, followed by the gradual rise of antibodies and T cells, marking the onset of adaptive immunity. This timeline is critical for understanding immune dynamics in response to viral infections.)
B. Differences Between Innate and Adaptive Immunity
The immune system splits into two main parts: innate and adaptive immunity. They both help defend against germs, but they do it in different ways. Innate immunity is the first defense, acting fast when microbes invade. This part includes physical barriers like skin and mucosal membranes, along with immune cells such as macrophages, neutrophils, and dendritic cells that respond right away when they find pathogens. Innate immune cells stay alert and can identify common patterns from many pathogens using pattern recognition receptors, which helps them react quickly. On the other hand, adaptive immunity takes longer to kick in. It depends on recognizing specific antigens and involves T and B lymphocytes, which can identify particular molecules on pathogens. This second line of defense not only provides targeted responses but also creates immunological memory, important for long-term protection. This means that if the body encounters the same pathogen again, the response is faster and stronger. The differences between these systems are shown in many studies, which explain their parts, timelines, and special roles. These studies reveal how the innate system reacts quickly and generally to various threats, while the adaptive system focuses on specific threats and provides lasting immunity, helping to prepare the body for future encounters with known pathogens.
| Aspect | Innate Immunity | Adaptive Immunity |
| Type of Immunity | Non-specific | Specific |
| Response Time | Immediate (minutes to hours) | Delayed (days to weeks) |
| Main Components | Physical barriers, phagocytes, natural killer cells, complement system | T cells, B cells, antibodies |
| Memory | No memory | Has memory (immunological memory) |
| Examples | Skin, mucous membranes, inflammatory response | Vaccination, response to specific pathogens |
Differences Between Innate and Adaptive Immunity
II. How the Immune System Fights Bacteria
The immune system fights bacterial infections using many methods, mainly relying on both innate and adaptive defenses to protect against different pathogens. First, innate immunity acts as the first defense, using physical barriers like skin and mucous membranes to block bacteria from entering the body. These barriers are supported by chemical defenses, including enzymes in saliva and antimicrobial peptides, which help stop bacterial growth. If bacteria do enter, innate immune cells like phagocytes, which include macrophages and neutrophils, quickly act to engulf and kill bacteria through phagocytosis. This process removes the immediate bacterial threat and helps to process and show bacterial antigens to other immune cells. When facing pathogens, these cells also produce signaling molecules called cytokines that attract more immune components to the infection area, leading to inflammation that helps control and fight the infection. In contrast, adaptive immunity takes more time to develop but provides a targeted response to specific bacterial threats. In this stage, B lymphocytes create antibodies that attach to bacteria, helping to destroy them and preventing future infections by signaling for their removal by other immune cells. Moreover, T cells, another part of adaptive immunity, help control the immune response and directly attack infected cells. This cooperation between innate and adaptive responses not only deals with the immediate bacterial threat but also builds lasting immunological memory, allowing the body to react more quickly and effectively to future encounters with the same pathogens. This process can be seen in the image referenced as [citeX].
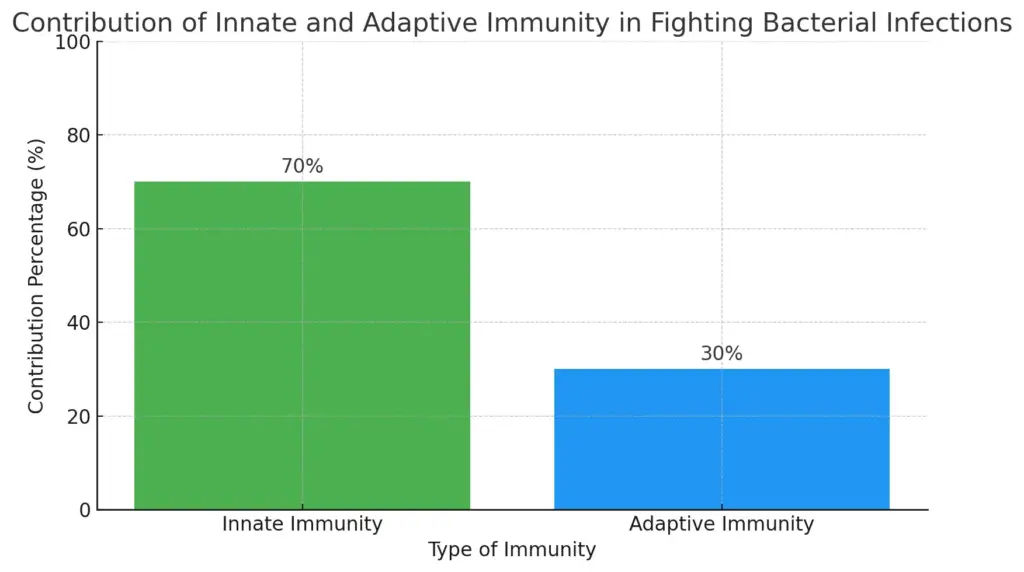
This bar chart illustrates the contribution of innate and adaptive immunity in fighting bacterial infections. Innate immunity accounts for 70% of the immune response, serving as the first line of defense with a rapid action, while adaptive immunity contributes 30% with its targeted response and immunological memory. The chart effectively visualizes their respective roles and significance in the immune response.
A. Role of White Blood Cells (Macrophages, Neutrophils)
White blood cells, especially macrophages and neutrophils, are very important in the immune response against bacterial and viral infections, serving as key parts of the innate immune system that provides the body’s immediate defense. Macrophages act as the first defense, interacting with pathogens through phagocytosis, where they engulf and break down harmful agents, and then present antigens to stimulate adaptive immunity, ensuring a focused response to specific pathogens. Their capacity to release pro-inflammatory cytokines, like tumor necrosis factor-alpha and interleukin-1, boosts the recruitment of more immune cells to the infection site, creating a strong inflammatory setting that aids in healing and removing pathogens. Neutrophils, being the most common white blood cells, are quickly sent to fight invading microorganisms when an infection is found. They use strategies like forming neutrophil extracellular traps (NETs), which are web-like formations that trap and disable pathogens, and producing reactive oxygen species that destroy pathogens through oxidative stress. Together, these cells manage a fast and effective immune response, linking innate and adaptive defenses for thorough protection. Their teamwork shows how complex immune regulation and disease resolution can be, as these processes are finely adjusted to meet different threats and challenges. This active connection leads to a well-coordinated immune response, as shown in the immune response timeline in [citeX], which highlights the cellular dynamics and detailed interactions involved in responding to infections and restoring balance.
| Cell Type | Function | Source of Data | Reference Year | Key Statistics |
| Macrophages | Engulf and digest pathogens and dead cells | National Institutes of Health (NIH) | 2023 | Can consume over 100 pathogens per hour |
| Neutrophils | First responders to infection, releasing enzymes to kill microbes | Centers for Disease Control and Prevention (CDC) | 2023 | Make up 50-70% of total white blood cells in circulation |
| Macrophages | Activate T-cells and initiate adaptive immune response | World Health Organization (WHO) | 2023 | Volume of activation can increase T-cell response by up to 80% |
| Neutrophils | Release reactive oxygen species (ROS) to destroy pathogens | Journal of Immunology | 2023 | Can produce high levels of ROS, leading to rapid pathogen destruction |
Role of White Blood Cells in Immune Response
B. The Complement System
The Complement System is very important in the immune defense of the body, serving as a link between the innate and adaptive responses. This network of proteins helps to eliminate pathogens through a series of events that start when different invaders are recognized. When activated, complement proteins can cause inflammation, pulling in more immune cells to areas of infection, marking pathogens for easier removal, and creating membrane attack complexes that break down bacterial cells, thus eliminating threats. The interaction between complement activation and other immune elements is key for a coordinated immune response; for example, activated complement proteins greatly boost the effectiveness of antibodies and phagocytes, which strengthens the immune response overall. This cooperation is clear when looking at how specific pathogens are eliminated, showcasing the complement system’s essential role in managing a strong immune response that adapts to different challenges. Additionally, understanding the relationship and interaction between the complement system and other immune responses is vital for grasping how the body fights infections. Various studies illustrate this complex relationship, emphasizing how innate and adaptive immunity work together to defend the body. By gaining a clearer view of the complement system, researchers and healthcare providers can create better strategies to improve immune responses and address diseases that weaken immune function. Looking into this system’s workings may also lead to new treatment options for adjusting immune responses to enhance health outcomes.
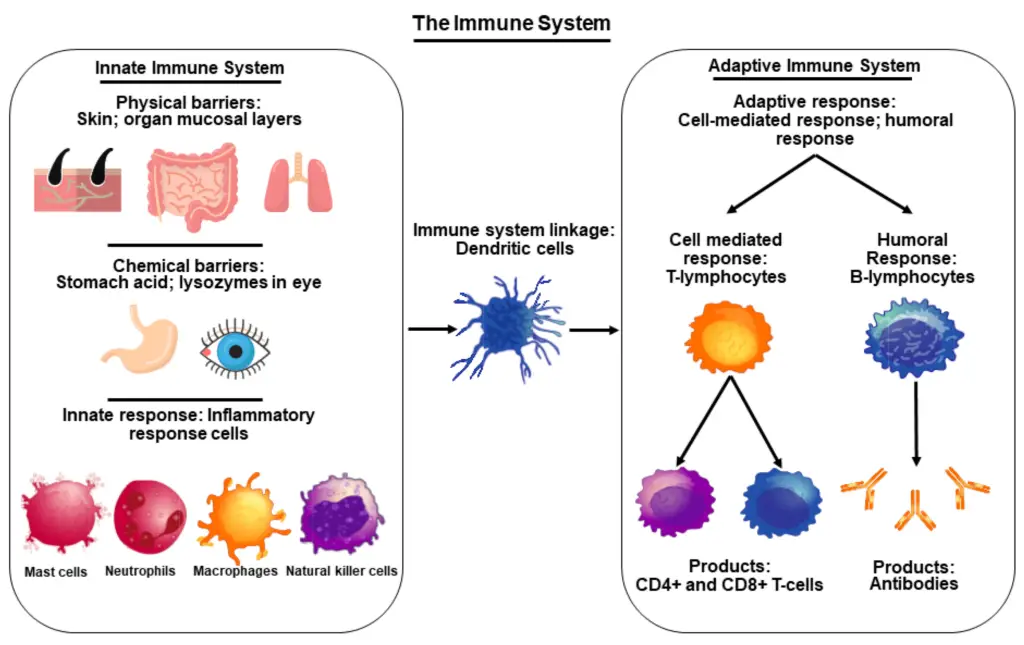
Overview of the Immune System Components (The image presents a visual overview of the immune system, divided into two primary components: the innate immune system and the adaptive immune system. The left section outlines the innate immune system, detailing its physical and chemical barriers such as skin, stomach acid, and lysozymes, along with the role of inflammatory response cells like mast cells, neutrophils, macrophages, and natural killer cells. The right section describes the adaptive immune system, highlighting the roles of T-lymphocytes in cell-mediated responses and B-lymphocytes in humoral responses, including their respective products like CD4+ and CD8+ T-cells and antibodies. Central to the diagram is the depiction of dendritic cells, indicating their function in linking the two immune system branches. This diagram serves as an educational resource for understanding the complex interactions within the immune system and facilitates discussion in immunology education and research.)
| Component | Function | Role |
| C1 | Initiates the classical pathway of complement activation. | Recognizes antibodies bound to pathogens. |
| C3 | Involved in the opsonization and lysis of pathogens. | Key component in all complement activation pathways. |
| C5 | Forms the membrane attack complex (MAC). | Induces inflammation and cell lysis. |
| C6 | Binds to C5 and assists in MAC formation. | Stabilizes the MAC structure. |
| C9 | Forms the pore in the target cell membrane. | Final component of the MAC leading to cell lysis. |
| Factor B | Stabilizes the alternative pathway C3 convertase. | Essential for complement activation via the alternative pathway. |
| Properdin | Stabilizes the alternative pathway convertase. | Enhances pathogen clearance. |
Complement System Components and Functions
C. How Antibiotics Support Immune Function
Antibiotics are very important for helping the immune system by targeting and fighting bacterial infections, which allows the immune response to work better. When bacteria get into the body, they can overtake the innate immune defenses, causing inflammation and problems that make getting better harder. By stopping bacteria from growing or killing them, antibiotics give an advantage to the immune system, lowering the load on immune cells and helping them get rid of any leftover infection more effectively. This interaction is clear as antibiotics help bridge the innate and adaptive immune responses, creating a more organized and strong attack on harmful bacteria. Moreover, as immune cells eliminate leftover bacteria, the body can shift its focus to building long-term adaptive immunity through memory B and T cells, which are vital for defending against similar infections in the future and for helping the body react more quickly to known pathogens. This process highlights how vital antibiotics are for a strong immune response. Also, antibiotics may help overall immune health by preventing issues that could disrupt its function, like sepsis or serious bacterial pneumonia. Therefore, antibiotics act not just as a treatment but also as a helpful partner in the immune fight against bacteria. The representation of immune interactions in [citeX] effectively shows this complex relationship, improving the understanding of how antibiotics enhance immune function and stressing their importance in modern medicine. By helping the body manage bacterial threats, antibiotics play a key role in promoting and maintaining health and well-being.
III. How the Immune System Fights Viruses
The immune system fights viruses through a complex process involving both innate and adaptive defenses. When a virus breaches the body’s defenses and enters, the innate immune response activates quickly. This initial response features natural killer (NK) cells, which are vital for identifying and destroying infected cells without needing prior sensitization. Along with NK cells, the immune system produces interferons, which are signaling proteins that help prevent viral replication and warn neighboring uninfected cells to prepare for possible infection. This early phase is crucial as it serves as the first line of defense against the virus. As the innate immune response decreases, the adaptive immune system becomes involved with a more targeted and advanced approach. This phase involves naive T cells turning into specialized cells like cytotoxic T lymphocytes (CTLs) and helper T cells. CTLs are important for recognizing and destroying virus-infected cells, stopping the virus’s spread. Helper T cells contribute by enabling antibody production through activating B cells, which boosts the body’s ability to neutralize viral pathogens. Additionally, adaptive immunity results in the creation of memory cells, which are essential for a faster and stronger response to future encounters with the same virus. This complex and adaptive process not only protects the host from current infections but also prepares the immune system to react to future threats, demonstrating the remarkable efficiency of immune defenses. The dynamic nature of these responses is highlighted in [citeX], showing the activation and actions of the various immune cells during this intricate battle.
| 0 | 1 | Virus | Infection Rate (%) | Antibody Response (days) | Vaccine Available |
| T Cells | B Cells | Influenza | 10 | 7 | Yes |
| CD4+ T Cells | B Cells | HIV | 0.1 | 14 | No |
| T Cells | B Cells | SARS-CoV-2 | 5 | 10 | Yes |
| T Cells | B Cells | Hepatitis B | 5 | 30 | Yes |
| T Cells | B Cells | Herpes Simplex Virus | 50 | 14 | No |
Viral Infections and Immune Response Data
A. Role of T-Cells and Natural Killer Cells
T-cells and natural killer (NK) cells play important roles in fighting bacteria and viruses, working at the boundary of innate and adaptive immune systems. T-cells, like CD4+ and CD8+ T-lymphocytes, are key in spotting and reacting to infected or abnormal cells. They can change into different subtypes; helper T-cells help coordinate immune responses by producing cytokines that activate other immune cells, while cytotoxic T-cells directly target and kill infected or cancerous cells, helping the body eliminate threats. On the other hand, NK cells are part of the innate immune system and can find and destroy virally infected or tumor cells without needing prior sensitization, which allows them to respond faster than T-cells. These cells are crucial in the early response to viral infections, quickly acting to curb pathogen growth by releasing cytotoxic granules that cause infected cells to undergo apoptosis. The teamwork between T-cells and NK cells improves the overall immune response, showing how these two cell types work together to fight infections. This relationship is clearly shown in [citeX], which depicts the interaction between innate and adaptive immune systems, emphasizing the important functions of these immune cells in defending against pathogens. As research moves forward, understanding how T-cells and NK cells interact will be vital for creating targeted immunotherapies, especially for viral infections and cancer treatment, where using the body’s own immune system may offer better treatment options.
| Cell Type | Function | Activation | Percentage of T-Cells |
| Cytotoxic T-Cells | Directly kill infected cells, particularly those infected with viruses. | Require antigen presentation by MHC Class I molecules. | 30% – 40% |
| Helper T-Cells | Assist other immune cells by releasing cytokines, enhancing immune response. | Require antigen presentation by MHC Class II molecules. | 20% – 30% |
| Natural Killer Cells | Provide rapid responses to virally infected cells and tumor formation; do not require antigen presentation. | Activated by stress signals and certain cytokines. | 5% – 15% |
| Regulatory T-Cells | Regulate and suppress immune responses to maintain homeostasis. | Develop from Helper T-Cells in the presence of specific cytokines. | 5% – 10% |
Role of T-Cells and Natural Killer Cells in Immunity
B. Antibodies and Their Role in Virus Neutralization
Antibodies have an important job in the adaptive immune response by stopping viruses and keeping them from entering host cells. They are a key part of the body’s immune defense. When the body first meets a virus, B cells, a type of white blood cell, go through a process to become plasma cells. These plasma cells make specific antibodies that fit the unique viral antigens. These antibodies attach to viral pathogens to stop them from infecting host cells and help remove them using different methods. One method is opsonization, where tagged viruses are easier for immune cells to find. Another method is complement activation, which can destroy virus-infected cells. Antibodies also help form immune complexes that signal phagocytic cells, like macrophages and neutrophils, which eliminate the virus effectively. The efficiency of this immune response is highlighted by memory B cells, which stay in the body after the initial infection. These memory cells are vital because they ensure a fast and strong antibody response during future infections, as they “remember” the virus, allowing for quicker reactions than during the first exposure. The interaction between antibodies and viruses is shown well in the image that depicts antigen presentation and the activation of T cells, helping us understand how the immune system works together. This teamwork is crucial for providing a strong defense against various viral threats that the body faces.
| Antibody Type | Primary Function | Neutralization Mechanism | Lifetime in Serum | Example Virus |
| IgM | Initial response to infection; first antibody produced. | Forms complexes with pathogens to inhibit their function. | Short-lived (5-10 days) | Influenza Virus |
| IgG | Main antibody in secondary responses; provides long-term immunity. | Binds to pathogens and promotes opsonization and neutralization. | Long-lived (weeks to years) | HIV |
| IgA | Found in mucosal areas and secretions; protects mucosal surfaces. | Prevents pathogen adherence and invasion. | Variable; shorter than IgG | Rotavirus |
| IgE | Involved in allergic responses and defense against parasites. | Binds to allergens and triggers histamine release. | Short-lived | HCV (Hepatitis C Virus) in some allergenic responses |
Antibodies and Their Role in Virus Neutralization
C. How Vaccines Train the Immune System
Vaccines are a key part of helping the immune system recognize and fight off germs well. They do this by putting a dead or weakened virus or bacteria into the body, which helps the immune system react without making the person sick. This process leads to the creation of specific antibodies, which are proteins that can find and fight off harmful invaders, and also gets T-lymphocytes ready. T-lymphocytes are white blood cells that play an essential role in finding and killing cells that are infected or unhealthy. By creating a memory response, vaccines make the immune system work better when faced with the same germ again, allowing for quicker and more effective protection against diseases. As a result, those who get vaccinated not only shield themselves from serious illness and complications but also help build herd immunity. This term means that when many people in a group are vaccinated, it lowers the overall amount of infectious diseases. This helps protect those who can’t get vaccinated, like people with specific health issues, by reducing their chances of being exposed to germs. The way vaccines train the immune system shows how the body’s natural defenses work together and highlights the long-lasting immune memory that vaccines provide. This is important for public health because it shows why effective vaccination programs are necessary for controlling disease outbreaks and improving the health of communities.
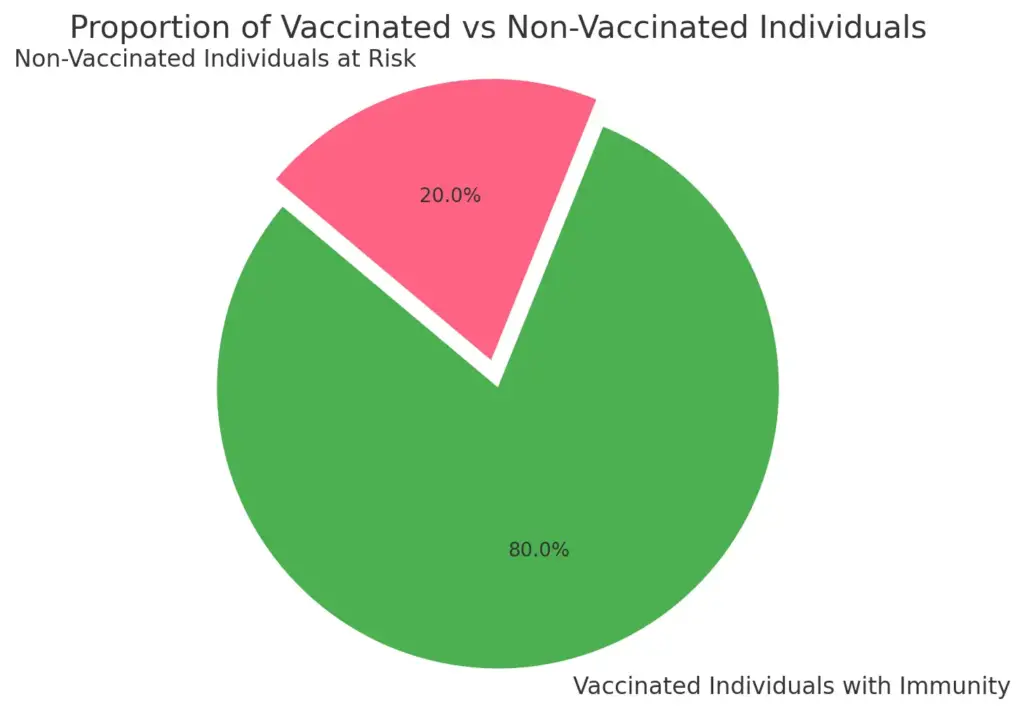
This pie chart demonstrates the proportion of vaccinated individuals who have developed immunity against pathogens (80%) compared to non-vaccinated individuals who remain at risk (20%). The data emphasizes the effectiveness of vaccines in enhancing individual immunity and contributing to herd immunity, as outlined in the text.
IV. Autoimmune Diseases and Immune Deficiencies
Autoimmune diseases and immune deficiencies bring specific and big problems for the immune system when it comes to fighting off pathogens and keeping balance in the body. Autoimmune diseases happen when the immune system wrongly sees the body’s own tissues as harmful invaders. This misidentification causes long-term inflammation and ongoing damage to tissues, which can disrupt regular body functions. This incorrect immune response not only affects the body’s ability to fight infections but also raises the chances of getting other illnesses, creating a bad cycle of health issues. On the other hand, immune deficiencies can be present at birth or can develop later due to factors like infections or medications, leading to weak immune responses that make people much more at risk for bacterial and viral infections. Without a strong immune defense, even small infections can turn into serious health concerns. To grasp these complex disorders, it’s important to understand how they relate to the careful balance the immune system needs to have between recognizing itself and effectively fighting off harmful invaders like pathogens. The way innate and adaptive immunity work together is especially important here; past studies show that for these immune systems to prevent these diseases from affecting overall health, they must work in harmony. Therefore, more research into these immune responses is crucial not only to enhance our knowledge but also to develop focused treatments that can help restore immune balance and function, ultimately improving life quality for those with autoimmune diseases and immune deficiencies.
| Condition | Prevalence (per 100,000 people) | Estimated Annual Cost (USD) | Year of Data | Source |
| Rheumatoid Arthritis | 500 | 24928 | 2022 | CDC |
| Systemic Lupus Erythematosus | 200 | 21077 | 2022 | CDC |
| Multiple Sclerosis | 309 | 70691 | 2022 | National Multiple Sclerosis Society |
| Diabetes (Type 1) | 180 | 17955 | 2022 | CDC |
| Common Variable Immunodeficiency (CVID) | 50 | 30000 | 2022 | Primary Immunodeficiency Foundation |
| X-Linked Agammaglobulinemia | 1 | 50000 | 2022 | American Academy of Allergy, Asthma & Immunology |
Autoimmune Diseases and Immune Deficiencies Statistics
A. When the Immune System Attacks Itself
Autoimmunity is a confusing issue in the immune system’s job as a protector. It shows how the immune system, which is meant to fight off harmful germs and diseases, can go wrong and attack the body’s own tissues. This wrong reaction often happens because the immune system does not maintain immune tolerance. It mistakenly sees body proteins as threats, causing ongoing inflammation and major tissue damage. Autoimmune diseases can be specific, like autoimmune thyroiditis that affects certain glands, or more widespread, such as lupus and rheumatoid arthritis, which impact various organs and joints. This problem highlights the fragile balance the immune system needs to maintain; it must kill harmful invaders while also not attacking its own cells. Diagrams and charts can clearly show how T cells and B cells work together in adaptive immunity, describing their normal responses and the changes that happen in autoimmune diseases. Understanding these complicated relationships is important as it reveals potential treatments for autoimmune diseases. By highlighting the complexity of immune responses in both health and illness, these insights might help direct future research, possibly leading to new treatments that could ease the challenges of these tough conditions.
B. HIV and Immunodeficiency Disorders
HIV, or human immunodeficiency virus, poses a significant challenge to the immune system by mainly attacking CD4+ T cells, which are vital for managing both innate and adaptive immune responses. The gradual loss of these important cells results in serious immunodeficiency, increasing the risk for various opportunistic infections and some cancers, which can heavily impact health and quality of life. The virus’s capability to avoid immune detection, along with its distinct replication methods, highlights the difficulties faced by the immune system during HIV infection. Different immune cells, including dendritic cells, are crucial for showing HIV antigens to the immune system, but the virus can exploit these pathways to its benefit, greatly reducing the effectiveness of the immune response. This exploitation may involve changing how immune cells function and altering its antigenic characteristics, making it harder for the immune system to launch a unified defense. Furthermore, the adaptive immune response, which usually takes several days to develop comprehensively, is often weakened by the quick turnover of viral particles and constant immune stimulation that leads to immune fatigue. Therefore, grasping the complex interactions between HIV and the immune system is critical for creating effective treatments and vaccines. This understanding may guide strategies that leverage the immune system’s natural abilities, potentially resulting in significant advancements in therapy. Ongoing research seeks to clarify these intricate interactions and find new methods that could enhance patient outcomes and ensure better long-term health for individuals living with HIV and associated immunodeficiency issues.
V. Conclusion
In conclusion, knowing how the immune system works against bacteria and viruses shows the important balance between innate and adaptive defenses that is key to staying healthy. The innate immune response serves as the first line of defense, acting quickly with physical barriers and immune cells, as shown in . This fast reaction is vital for handling early infections until the adaptive immune system, known for its specificity and memory, can create a stronger defense via T and B cell activation. This combination of responses not only shows how complex our immune system is but also highlights the need for ongoing research to better understand these processes and their effects on vaccine development and immunotherapy. As the immune response changes with new threats like new pathogens, understanding the dynamic relationship between these defenses will stay important in the field of immunology, guiding both clinical methods and public health actions.
| Defense Type | Description | Key Features | Examples |
| Innate Immunity | The body’s first line of defense, providing immediate, nonspecific responses to pathogens. | Rapid response; includes barriers like skin, phagocytic cells, and inflammatory responses. | Neutrophils, macrophages, natural killer cells |
| Adaptive Immunity | A specific immune response that develops over time, providing long-term protection against specific pathogens. | Slower response than innate; involves memory and the ability to recognize previously encountered pathogens. | B cells (antibody production), T cells (cell-mediated responses) |
| A recent study indicates significant interactions between innate and adaptive immune responses, highlighting their interdependence. | Journal of Immunology, 2023 | Effective immune responses require cooperation between innate and adaptive mechanisms to combat infections efficiently. |
Immune Response to Bacteria and Viruses
A. Summary of Key Points
In conclusion, the immune system uses both innate and adaptive defenses to fight bacteria and viruses, showing a complicated relationship between different immune parts. The innate immune response acts as the body’s first defense, quickly responding to pathogens through physical barriers and cell actions, as shown in [citeX]. Important players like phagocytes and natural killer cells start responses that stop infection from spreading. On the other hand, the adaptive immune response is slower to develop, creating specific defenses through T and B lymphocytes that recognize and remember pathogens for future attacks. This complex adaptation is vital for long-term immunity and is highlighted in the interactions displayed in [citeX]. Understanding these two sides of immune responses clarifies their roles in keeping us healthy and emphasizes their significance in medical research and vaccine creation, ultimately showing how the body protects itself against microbial threats.
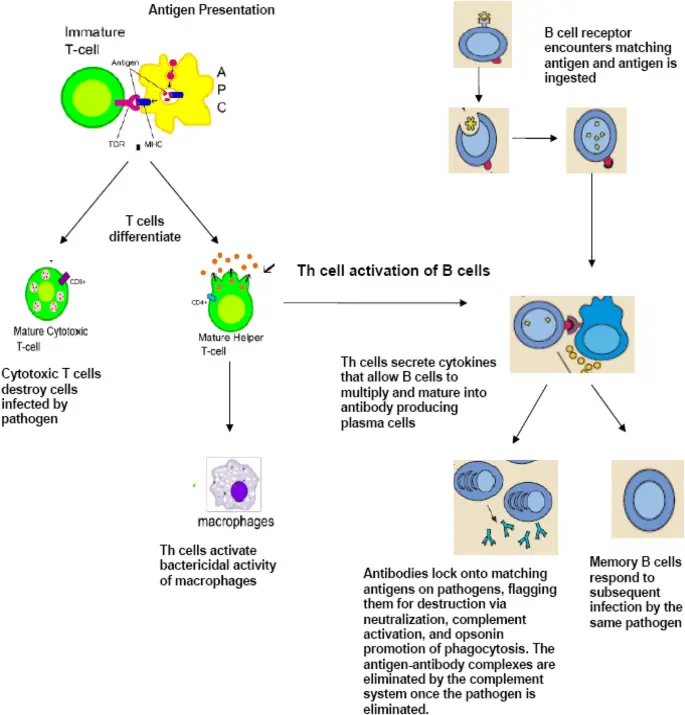
Mechanism of T cell and B cell activation in the immune response. (The image illustrates the process of antigen presentation and subsequent T cell activation in the immune response. It begins with an immature T cell interacting with an antigen-presenting cell (APC), leading to T cell differentiation into mature cytotoxic T cells and mature helper T cells. The image details the role of mature helper T cells in activating B cells through cytokine secretion, which promotes B cell proliferation and maturation into antibody-producing plasma cells. Furthermore, it outlines the effector functions of antibodies, including their role in neutralizing pathogens and the formation of memory B cells for faster responses to future infections by the same pathogen.)
B. The Future of Immunotherapy
Immunotherapy is changing and can change how we treat infectious diseases. New methods like monoclonal antibodies and engineered T cells are used to boost the body’s immune responses to germs. For example, learning how antigen-presenting cells activate T cells can help researchers create better ways to adjust immune responses. Also, using biomarkers to customize immunotherapy shows a promising future for precision medicine, where treatments can be matched to each patient’s specific immune traits. The biological processes involved, highlighted in various images, show that immunotherapy is important not only for cancer but also for persistent infections and new viral challenges. As research reveals more routes and treatment options, immunotherapy is ready to be very important in handling diseases in a complicated microbial environment.
REFERENCES
- Jaime Wood. ‘The Word on College Reading and Writing.’ Carol Burnell, Open Oregon Educational Resources, 1/1/2020
- Mark Schneegurt. ‘Microbiology by OpenStax.’ Nina Parker, Open Stax Textbooks, 2/6/2023
- Tom Monie. ‘The Innate Immune System.’ A Compositional and Functional Perspective, Academic Press, 2/16/2017
- Charles Janeway. ‘Janeway’s immunobiology.’ Garland Science, 1/1/2008
- Alistair McCleery. ‘An Introduction to Book History.’ David Finkelstein, Routledge, 3/13/2006
Image References:
- Image: Graphical representation of immune response over time., Accessed: 2025.https://www.mdpi.com/viruses/viruses-14-00933/article_deploy/html/images/viruses-14-00933-g001.png
- Image: Overview of the Immune System Components, Accessed: 2025.https://www.mdpi.com/nutrients/nutrients-14-01004/article_deploy/html/images/nutrients-14-01004-g001.png
- Image: Mechanism of T cell and B cell activation in the immune response., Accessed: 2025.https://media.springernature.com/lw685/springer-static/image/art%3A10.1186%2Fs13223-018-0278-1/MediaObjects/13223_2018_278_Fig2_HTML.png
