Impact and Economic Importance of Plasmodium: A Detailed Study
Delving into the universe of microscopic organisms, the narrative of Plasmodium reveals the profound consequences it holds within our socio-economic structures. Plasmodium, a potent parasite transmitted by mosquitoes, is responsible for instigating malaria, a menacing disease that severely deteriorates human health.
Instead of its minuscule biological footprint, the total ramifications it inflicts on the economic sphere are monumental. The subsequent paragraphs of this composition will navigate through the life cycle of this parasite and its correlation with malaria, the resultant economic implications, the straining effects on the public health system, and finally, the cost-effectiveness of curative and preventative measures currently employed to combat this disease.
Overview of Plasmodium
An Insight into the Complex World of Plasmodium and Its Intricate Life Cycle
The brilliance of the natural world is revealed in myriad forms, one of which is a minuscule, parasitic protozoan responsible for a billion-dollar global health problem: malaria. This resistor is Plasmodium, a genus that subjected the medical world to strapping challenges. Delving into its intriguing life cycle endows us with profound insights into the parasite’s stupendous survival strategy.
Plasmodium species – including P. falciparum, P. vivax, P. ovale, P. malariae, and P. knowlesi – are highly evolved parasites that have adapted to make two different hosts, namely, female Anopheles mosquitoes and human beings, their temporary abode. The Plasmodium’s life cycle embodies a rigorous example of the evolutionary perfection of parasitism.
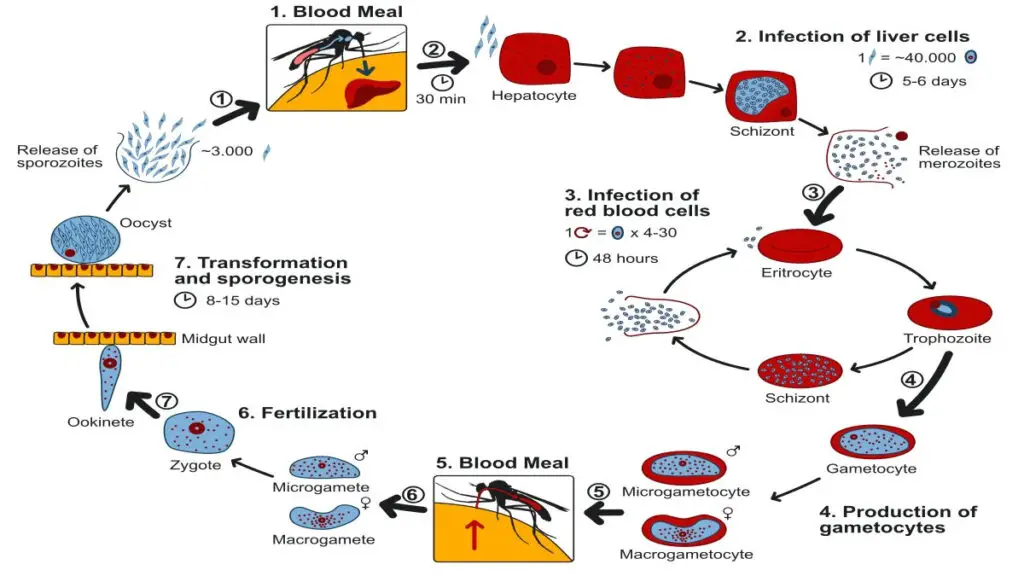
In pursuit of its survival and propagation, Plasmodium commences its journey inside a feeding female Anopheles mosquito where it exists as a sporozoite. Entering a human host during a mosquito blood meal, the sporozoite traverses into the hepatic cells to trigger the liver stage. Amidst the safe haven of hepatic cells, they transform into merozoites – a process known as schizogony – hence increasing in number.
In the next phase, merozoites are passed into the bloodstream, where they rapidly invade the red blood cells (RBCs). Within the safe confines of the RBC, the merozoite rapidly matures into a trophozoite, which further propagates by schizogony, resulting in the release of more merozoites. This relentless multiplication causes RBC rupture with consequent cycles of fever in the human host.
Simultaneously, some merozoites deviate from this asexual cycle and transform into gametocytes – the sexual stage. When an Anopheles mosquito feasts on an infected individual’s blood, these gametocytes are ingested, giving rise to male and female gametes in the mosquito’s stomach. Fusion of these gametes results in zygotes that differentiate into ookinetes, finally maturing into oocysts at the stomach lining.
Inside the oocysts, thousands of sporozoites are developed, which later migrate to the mosquito salivary glands, thus primed and ready to initiate a new infection cycle in another human host.
Understanding Plasmodium’s life cycle is pivotal in unravelling the enigma of its pathogenesis – the puzzle malaria researchers are enthusiastic about solving. This insight has not only elucidated the evolutionary conservation of life-cycle stages but also proved cardinal in the identification of potential drug targets.
Upon studying Plasmodium’s life cycle, we come to an understanding that this parasite has evolved extraordinarily robust mechanisms to ensure its survival and transmission – a testament to nature’s relentless power and dexterity.
However, with our continuous formidable endeavours in research and technology, hope is nurtured to combat this river horse of a malaria parasite, turning our knowledge into power, for global health improvement and sustenance. Moreover, appreciating the beauty of this intricacy lends a unique philosophical touch, enriching our perception of the amazing diversity of life.
Plasmodium and Malaria
In delving deeper into the link between Plasmodium species and malaria, one can glean insightful revelations concerning the relationship these microorganisms have with human hosts.
While the focus so far has largely emphasized the Plasmodium life cycle, its multiple hosts, and the pathogenic manifestations, a further illumination of the molecular mechanisms and adaptive mutations this genus executes will facilitate a more comprehensive understanding of how malaria emerges and evolves.
On the molecular level, Plasmodium has a unique and sophisticated way to infiltrate the human immune system. Different species of Plasmodium have been found to express a versatile set of molecules known as Plasmodium falciparum Erythrocyte Membrane Protein 1 (PfEMP1). It is noted for its antigenic variation, enabling Plasmodium to evade antibodies, providing an avenue for continued infection. Continual modification of these molecules contributes to the parasite’s adeptness at deceiving the host’s defensive mechanisms, enabling the cycle of infection to be perpetuated effectively.
Furthermore, Plasmodium’s adaptive mutation, referred to as antimalarial resistance, is a critical factor in the struggle against malaria. For instance, Plasmodium falciparum and Plasmodium vivax have developed resistance to different antimalarial drugs such as chloroquine and sulfadoxine-pyrimethamine. These mutations occur in the parasite’s genome and lead to structural and functional alterations in its metabolic pathways, conferring survival advantages to these microorganisms in medicinal environments. The emergence and spread of antimalarial-resistant Plasmodium species further complicates the disease’s global management.
Plasmodium’s genomic complexity renders further possibilities of unforeseen surface antigens and metabolic pathways being discovered, enriching the existing understanding of how these parasites function, adapt, and survive. This simultaneously encapsulates the challenging predicament posed by Plasmodium species towards curbing the burden of malaria.
Plasmodium’s complex and dynamic interaction with both its mosquito vector and human counterpart necessitates exhaustive research and innovative technological advancements for its grand reveal and eventual control. Ground-breaking technologies such as genome sequencing, proteomics, and genetically engineered mosquitoes are paving the way for an era of new discoveries and strategies. Meanwhile, potential vaccines offer glimmers of hope, though they must be scrutinized extensively for their efficacy, safety, and affordability.
Indeed, as one ventures further into the intricate realms of Plasmodium and its manifold implications for malaria, endless questions emerge. The push and pull between Plasmodium’s survival strategies and humanity’s attempts to counteract them paints a fascinating yet dimly understood landscape.
As scholars endeavor to peel back layers of this complex organism and malaria’s reality, one can only marvel at the biological sophistication displayed, enriching our understanding of microorganism-host interactions and their roles in the theatre of life.

Economic Consequences of Malaria
The economic implications of malaria, a fatal disease caused by the Plasmodium parasite, extend to the intricate networks of local, national, and global economic landscapes.
Malaria, historically entrenched in low and middle-income countries, fosters a cyclical pattern of poverty. Countries grappling with a high disease burden face a reduction in their Gross Domestic Product (GDP). Measurable economic loss is conspicuous in terms of healthcare costs, not just in providing direct medical treatment but also through preventive measures such as vector control and vaccination programmes. It’s essential to factor in the costs related to equipment, drugs, and human resources for delivery and implementation.
Indirect costs associated with malaria also mount up extensively. These encompass reduced labour productivity emanating from illness or death. Lost educational opportunities occur through school absenteeism due to illness, either affecting students directly or family circumstances related to malaria. This truncates the skill development and potential productivity of future workforce generations, maintaining a vicious cycle of disease-induced poverty.
Malaria also detrimentally affects tourism, a major economic pillar in many endemic countries. Fear of contracting the disease affects tourist arrival numbers and their expenditure, undermining local businesses and service industries. Investor confidence, especially in labor-intensive sectors, might abate in regions with high malaria prevalence, stunting the growth of local industries.
National economies are further strained when malaria drains considerable portions of public health budgets, diverting funds from other developmental sectors. Meanwhile, on a macroeconomic level, spending on malaria controls can sometimes increase a country’s debt burden, influencing economic policies and fiscal adjustments. This economic albatross has profound implications for regional stability and broader development efforts—an impact that reverberates across international borders.
However, the fight against malaria also promises significant economic upsides. Studies conclude that successful malaria control contributes positively to economic growth. For instance, agricultural productivity increases can lead to wider economic improvements and poverty reduction, while improved child health could increase school attendance and later earnings, breaking the cycle of poverty.
Significant investment in malaria research and product development over the past two decades has been a boon, bringing forth novel drugs, diagnostics, vector control technologies, and potential vaccines. This exemplifies how science and technology can drive economic growth, spur entrepreneurship, and create jobs. Notably, it also underlines the inextricable link between global health and the economy.
In essence, malaria’s economic toll moves beyond pure dollars and cents, affecting core development indices, intergenerational equity, economic policies, and global stability. Yet it also vividly emphasises the need and potential for continued research, innovative thinking, and determined actions to counteract Plasmodium’s relentless assault. Recognizing malaria’s economic impact is pivotal to informing efficient resource allocation, policy decisions, and anticipatory planning, ensuring strides toward malaria’s eradication and an economically healthier future.

Impact on Public Health System
When an outbreak of malaria occurs, it significantly affects the mechanisms of the public health system. The strain is particularly evident in resources, infrastructure, and manpower—key pillars that form the foundation of any well-functioning healthcare system. The high increase in demand for healthcare services, along with the need for immediate and effective responses, can lead to over-extension and potential crises within the health sector.
An upsurge in malaria cases requires rapid diagnosis and effective treatment to control the spread of the disease. This need can lead to an acute shortage of diagnostic kits, proper medication, and hospital beds, thereby heavily taxing already strained healthcare systems, especially in regions that are economically challenged or lack resources.
A large-scale malaria outbreak necessitates astute surveillance and clinical case management. The collection, analysis, interpretation, and dissemination of health data is pivotal in controlling and preventing future outbreaks. However, the surge in cases can overwhelm surveillance systems, healthcare professionals, and diagnostic laboratories, compromising the capacity to monitor and effectively respond.
Meanwhile, overburdened healthcare providers are at risk of exposure to the disease. This could aggravate the situation by reducing the number of healthcare providers available to care for patients, further overwhelming the health system.
Importantly, the health system itself becomes central in the fight against malaria, playing a decisive role in intervention strategies such as vector control programmes. The increased need for these programmes puts additional strain on the system, adding to the expectations and responsibilities of public health officials and workers.
The control, prevention, and eradication of malaria do not happen in isolation. Their success depends heavily on effective community mobilisation and public awareness campaigns. Thus, the health system also has to ensure mass communication and community-based efforts, expanding its role beyond direct healthcare provision.
Interestingly, looking beyond immediate health impacts, a malaria outbreak can also have profound socio-economic effects. Workforce productivity decreases due to illness, as does school attendance, resulting in a future workforce that is less educated. The economy becomes strained, and addressing these indirect consequences also falls within the health system’s remit.
In conclusion, a malaria outbreak significantly challenges the working of the public health system both directly and indirectly, necessitating a Herculean effort in diagnosis, treatment, surveillance, preventive measures, community mobilisation, and socio-economic mitigation. The anticipation of an outbreak should inspire proactive strengthening of public health infrastructure and systems, paving the way for faster, more effective responses. The fight against malaria is not just about combating a disease; it’s about bolstering a public health system’s resilience and capacity to protect society’s health and well-being.

Cost-Effectiveness of Malaria Control Measures
Analyzing the Effects of Malaria on Public Health Systems
Delving deeper into the impacts of malaria, it emerges as not only a severe health crisis but a contributing factor in resource strain. The resources that constitute public health systems can be categorically divided into infrastructure, manpower, and health commodities like drugs and diagnostic tools.
In regions with a high prevalence of malaria, these resources are inordinately focused on combating the disease. Hospitals and dispensaries are perennially filled with patients suffering from malaria, causing an increase in demand for healthcare services. This heightened demand, often beyond the capacity of existing healthcare infrastructure, leads to potential crises in health sectors.
Moreover, the rise in malaria cases causes a significant surge in the need for diagnostic kits, medication, and hospital beds. At times, when malaria simultaneously strikes large populations, shortages in these resources, pivotal to fighting the disease, can become pronounced. Shortages also significantly impact health systems by overwhelming surveillance systems, healthcare professionals, and diagnostic laboratories.
Increased demand significantly burdens healthcare providers. The impact goes beyond physical exhaustion to increased risk of exposure to the disease. Notably, the decrease in the number of healthcare providers available to treat conditions other than malaria spells disaster for overall communal health.
The role of the public health system extends beyond treating those affected to preventative measures such as running vector control programs. These programmes involve concerted efforts to reduce the mosquito population and lower the transmission rate of Plasmodium. Such preventative programmes become crucial to the sustenance of a community battling recurring malaria bouts, and their implementation rests heavily on the strength and efficiency of the public health system.
Part and parcel of prevention strategies are community mobilization and public awareness campaigns. Public health systems must engage the masses in conversations about the disease, its transmission, prevention, and control. These programmes, when carried out effectively, resulting in better compliance with mosquito avoidance measures, contributing to a reduction in infection risk.
In light of these points, the socio-economic effects of a malaria outbreak become concrete: less work is completed, productivity declines, and overall development is hampered. These impacts reiterate the need for strengthening public health infrastructure and systems and ensuring they’re equipped to respond more quickly and effectively to outbreaks.
Essentially, the fight against malaria is invariably linked to the overall health and development of affected communities. It reveals a crystal-clear interconnection between public health, socio-economic stability, and overall development. Thus, investing in malaria control measures isn’t merely a response to a health crisis; it is an economically sound decision with the potential for long-lasting socio-economic benefits.

The evaluation of Plasmodium and its association with one of the world’s deadliest diseases offers a glimpse into the labyrinth of medical, socio-cultural, and economic implications. Like an insidious adversary, this parasite happens to drain our economy, refurbishing productivity landscapes, reshaping healthcare models, and redrafting public health strategies.
Challenging the might of our systematic reforms, it emphasizes the impulse for research and development to invent a resilient intervention blueprint. It’s a potent reminder that something as seemingly insignificant as a single-celled parasite can trigger an enormous impact on civilization.
The journey of understanding Plasmodium and its implications on human existence and our socio-economic fabric continues, urging us to strategize well against our microscopic antagonist and create sustainable health infrastructure for the present and our future generations.

